Cancer and Cancer Immunotherapy
Cancer and Cancer Immunotherapy
Cancer is a group of disease that is caused by multiple alterations of normal genes leading to abnormal growth of cells. Typically, a type of gene, also known as “Oncogenes”, is found overexpressed and its products actually interfere with metabolic pathways of the cell causing the cells to multiply rapidly. Additionally, mutation in the tumour suppressor genes, leading to its functional loss, also strengthens the multiplication (1). Alteration in telomerase activity, hypo-oxic cellular nature and aggregation of immune cells around the cancer cells, all of which in worst case leads the localised multiplication to metastatic nature are typical events involved in a cancer. Furthermore, origin of mutation at different stages of development of cell caused the cancer cells of same type to be highly heterogeneous. Apart from that, these cancer mutants are different with the location and type of cells involved causing inter-tumoral heterogeneity (2, 3). For these complexities presented in a disease, treatment of cancer is causing humiliation in scientific community despite high investment on research in the field.
Various studies have been done to reduce the burden of such a group of disease. Different types of treatment methods have been developed, however, the techniques have gained limited success in curing the condition. Chemotherapy, hormonal therapy, radiotherapy and to some extent gene therapy is being used in treatment of the disease (2). Despite billion dollar investments, effectiveness of treatment method used to treat cancer is improving slowly. The main reason for such slow growth rate for effectiveness of treatment methods is due to the various factors and characters of cancer cells described earlier. Intra and Inter-tumour heterogeneity, rapid multiple mutations, metastasis, non-specific treatment methods and drug resistances are major factors associated with ineffective cancer therapy.
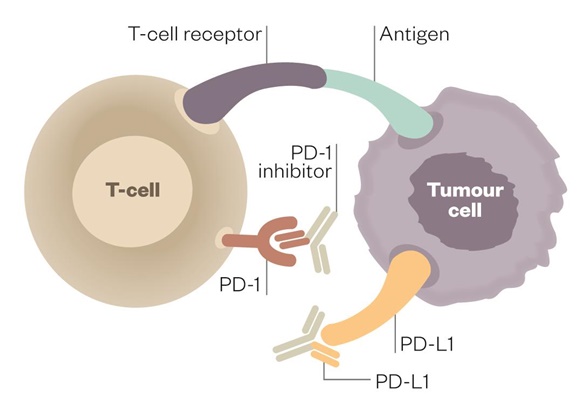
Following the toughest quest of finding proper way to address the burden of cancer, scientists found immune checkpoints, where immune molecules can be manipulated to ameliorate the situation. These cancer cells were found to express PDL1 and PDL2 ligands, which interacts with PD1 surface molecules of CD8+ T-Lymphocytes (4). However, the belief that cancer cells weren’t detected by host immune has been refuted, these molecules or molecular patterns were found to turn off the immune cells causing them ineffective. After reviewing the PD1 pathway in cancer development, it was predicted that targeting the PD1 pathway has promising pathway in treatment of the disease (5). From then, Scientists are trying to inhibit or disrupt the interaction between the two molecular patterns and striving to make the host’s immune system capable to fight against the abnormal cells. A study done to limit cancer showed the efficient treatment evidenced by sufficient reduction in tumour cells after blocking PD1 by using anti-PD1 agent called pembrolizumab (4). In this study, nearly fifty cancer (Melanoma) patients with metastatic nature were subjected to different analytical tests – multiplex immunofluorescence, immunohistochemistry and next generation sequencing for detecting receptors on cytotoxic T-lymphocytes. And, from the study, it was concluded that blocking PD1 pathway requires previously deregulated CD8+ T cells, inactivated by interaction of these cells with the cancer cells.
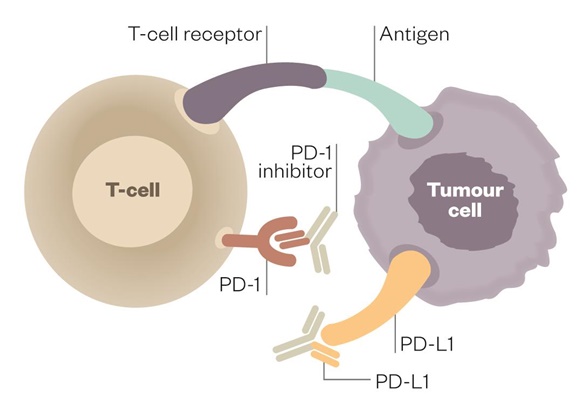
Figure: Therapeutic Antibodies blocking both PD1 and PDL1 in Cancer microenvironment. [Source: Pharmaceutical.com].
In another similar study, 41 patients with various types of cancer were analyzed for the expression of PDL1 & PDL2 in tumor cells and PD1 in T cells. From the study, PD1 suppression was concluded to be a major strategy in treating cancer, which was evidenced by presence of tumor PDL1 expression in immune active tumor microenvironment (6). However, the study showed varying expression levels for different disease types. Furthermore, in non-small cell lung cancer, melanoma and renal cell carcinoma, expression of PDL1 was higher suggesting the possible effectiveness of PD1 blockade mechanism. In this study, a therapeutic anti-PD1 antibody – Nivolumab has been used to treat the patients.
In this way, different antibodies are being developed and used in cancer therapy, using the advancements of protein technology. Currently, two anti-PD1 checkpoint inhibitors described earlier and a anti PDL1 antibody has been developed in the quest of fighting cancer (7). This modification helped host immune to bypass the interaction of PD1 and PDL1 and ultimately increased immunity against cancer. Studies done recently are corroborating the concept and the method is gaining more popularity in treatment of cancer. Some recent studies are also indicating superior suppression of tumour cells when the method to inhibit PDL1-PD1 interaction is applied in conjunction with some cancer vaccines (8). This treatment method, where immune molecules are involved in treatment of cancer, is now referred to as Cancer Immunotherapy and is treated as a major advancement in treatment of cancer.
However, some other scientists even thought to knock out the gene encoding the PD1 in the patients, modifying the immune cells genetically in cancer patients (9). The idea of knocking out of gene was possible only after the advent of site-specific endonucleases capable of causing double stranded breaks on the nucleic acids.
References
- White MK, Khalili K. CRISPR/Cas9 and cancer targets: future possibilities and present challenges. Oncotarget. 2016;7(11):12305-17.
- Grizzi F. Cancer heterogeneity and drug metabolism: What we know and what we need to know. Future Oncology. 2016;12(11):1317-9.
- Shoag J, Barbieri C. Clinical variability and molecular heterogeneity in prostate cancer. Asian Journal of Andrology. 2016;18(4):543-8.
- Tumeh PC, Harview CL, Yearley JH, Shintaku IP, Taylor EJM, Robert L, et al. PD-1 blockade induces responses by inhibiting adaptive immune resistance. Nature. 2014;515(7528):568-71.
- Hamid O, Carvajal RD. Anti-programmed death-1 and anti-programmed death-ligand 1 antibodies in cancer therapy. Expert Opinion on Biological Therapy. 2013;13(6):847-61.
- Taube JM, Klein A, Brahmer JR, Xu H, Pan X, Kim JH, et al. Association of PD-1, PD-1 ligands, and other features of the tumor immune microenvironment with response to anti-PD-1 therapy. Clinical Cancer Research. 2014;20(19):5064-74.
- Sgambato A, Casaluce F, Sacco PC, Palazzolo G, Maione P, Rossi A, et al. Anti PD-1 and PDL-1 immunotherapy in the treatment of advanced non-small cell lung cancer (NSCLC): A review on toxicity profile and its management. Current Drug Safety. 2016;11(1):62-8.
- Nowicki TS, Anderson JL, Federman N. Prospective immunotherapies in childhood sarcomas: PD1/PDL1 blockade in combination with tumor vaccines. Pediatric Research. 2016;79(3):371-7.
- Su S, Hu B, Shao J, Shen B, Du J, Du Y, et al. CRISPR-Cas9 mediated efficient PD-1 disruption on human primary T cells from cancer patients. Scientific Reports. 2016;6.
- http://www.pharmaceutical-journal.com/news-and-analysis/feature/immune-checkpoint-inhibitors-bring-new-hope-to-cancer-patients/20067127.article
Nice
Very nice Explanation